Cervical Cancer and Uterine (Body) Cancer – What is the Difference?
Although cervical cancer and uterine (body) cancer develop only a few centimetres apart, there are big differences in the cause of the disease. Therefore, the fields of research and treatment are also fundamentally different. This article will explain the differences, for a better understanding.
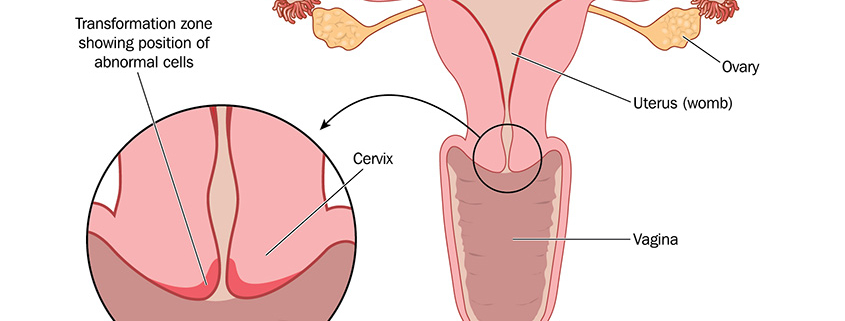
First, anatomy, in order to be able to better classify where both types of cancer originate: the uterus consists of the cervix, which ends at the lower end in the uterine orifice. The uterine body (corpus uteri) is connected to the upper end of the cervix. Cervical cancer develops in the cervix, only a few centimetres away from the uterus, where uterine (body) cancer develops.
Uterine Cancer – Factors, Occurrence and Symptoms
Uterine cancer (endometrial carcinoma, womb cancer, or corpus carcinoma) usually originates from the cells of the uterine mucosa. There is the very common oestrogen-dependent type I and the rare oestrogen-independent type II. Hereditary factors, overweight, diabetes and a long oestrogen influence (mostly caused by hormonal imbalances) favour uterine cancer. Uterine cancer usually occurs in older women. The average age is 69, and there is no regulated screening, as there is no cost-effective and reliable procedure for early detection.
While cervical cancer does not necessarily have symptoms, or they appear very late, uterine cancer usually has unusual bleeding at an early stage. If the patient goes to the doctor immediately and the bleeding is indeed a symptom of uterine cancer, there is a good chance of recovery. The uterus, fallopian tubes and ovaries may then be removed by surgery. If the cancer is more advanced, further treatment is necessary.
Cervical Cancer – Cause, Prevention, Treatment
Conditions are completely different in the case of cervical cancer: this disease develops over many years as a result of infection with certain strains of human papillomavirus (HPV). Through regular preventive care, preliminary stages, so-called dysplasias, can be detected and treated. Preliminary stages do not necessarily lead to the outbreak of cervical cancer. They may also regress. In any case, they must be observed. If a procedure is necessary, it is usually the so-called conisation, which aims at removing the carcinoma completely. As patients are often women of childbearing age, it is important to remove as little of the cervix as possible to avoid complications in possible later pregnancies.
Although cervical cancer (cervical carcinoma) and uterine cancer (endometrial carcinoma) develop only a few centimetres apart, they are two completely different types of cancer with different courses, symptoms and treatments. Particularly, cervical cancer is preventable: anyone who goes for regular cervical check and is vaccinated has a very low risk of developing it.
In summary, the following table provides an overview of both types of cancer:
| Cervical cancer (cervical carcinoma) | Uterine cancer (endometrial carcinoma) | |
| Frequency | 500.000 worldwide | 382 069 worldwide |
| Average age of patients | 34 (for early-stage carcinoma)
53 (for advanced carcinoma that has already spread to other tissue) |
69 |
| Main cause/trigger | Human papillomaviruses (HPV) | Genetic factors, overweight, diabetes, hormonal imbalances |
| Symptoms | Not necessarily. There may be pain during sexual intercourse, discharge or bleeding (in late stages) | Bleeding (in early stages), other symptoms occur in later stages |
| Prevention | HPV vaccination, screenings | Healthy lifestyle |
| Early detection | Organized screening, regulated by law | No screening program. Examination (ultrasound or uterine endoscopy) can be performed as an individual health service (IGeL) |
| Duration of development | Over a number of years | |
| Treatment | Observation and tests for preliminary stages, conisation for cancer (surgical procedure in which a conical piece of the cervix is removed) | Surgical procedure (removal of the uterus, fallopian tubes and ovaries), additional treatment in case of advanced stages |

 Blamb/Shutterstock.com
Blamb/Shutterstock.com

 oncgnostics GmbH
oncgnostics GmbH
 Eberhard Schorr / oncgnostics GmbH
Eberhard Schorr / oncgnostics GmbH
